Bone and Joint Infections
Presentation
Bone and joint infections can have a wide spectrum of presentations including
- Septic arthritis- Joint infections
- Osteomyeltis (Bone infection)- Acute or Chronic
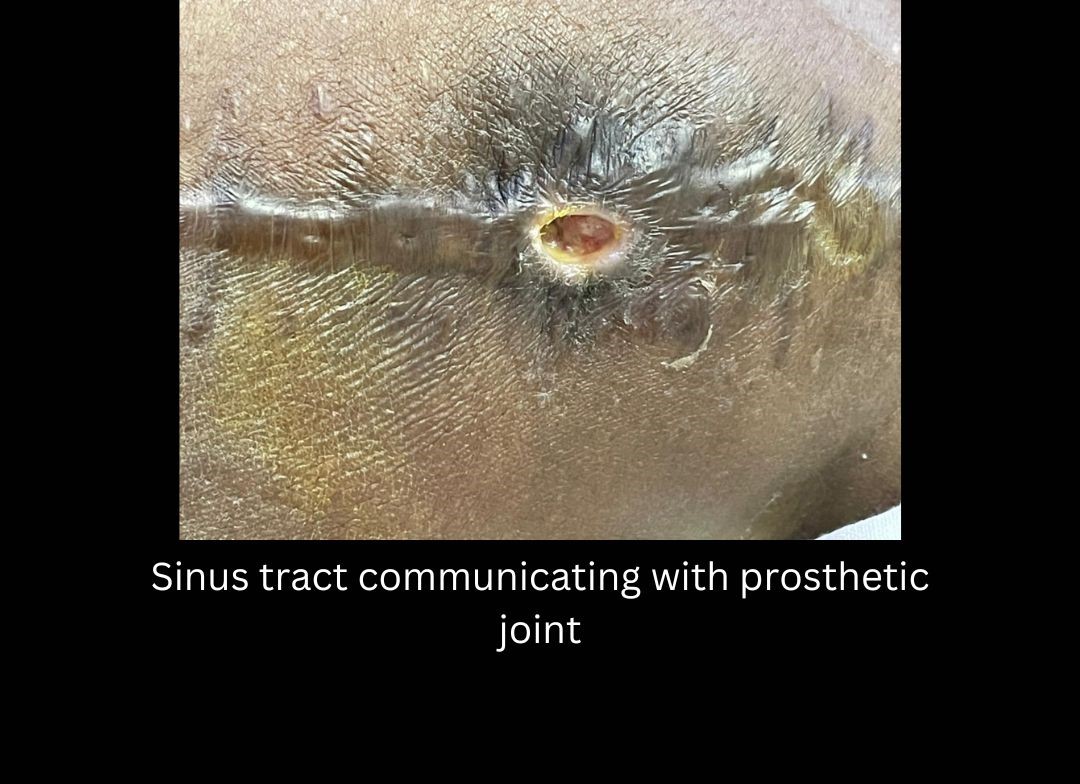
- Prosthetic Joint Infections (PJI)- Infection after Joint replacement Surgery
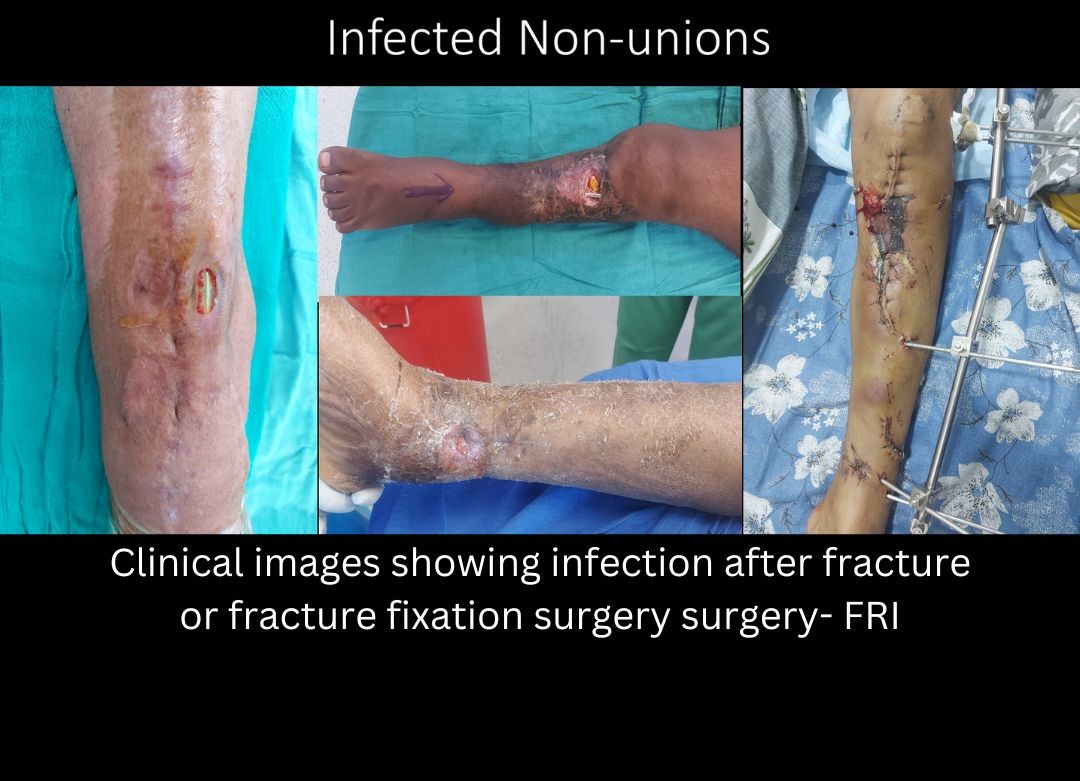
- Fracture related infection (FRI)- Infection after fracture fixation.
- Diabetic Foot
Acute infections like septic arthritis/ acute osteomyelitis are relatively easy to diagnose. An early diagnosis in such conditions is the key to a successful outcome. They warrant urgent surgical intervention. Presenting features include fever, severe pain, tenderness, erythema, or redness at the site and raised inflammatory markers on blood examination. Chronic infections on the other hand may be difficult to diagnose. The presence of a sinus tract communicating with a prosthetic joint or fracture fixation implant confirms the diagnosis of chronic infection. On other occasions the diagnosis may not be so apparent. Indirect evidence of infections include persistent pain, swelling, implant loosening, osteolysis and presence of low grade fever.
Diagnosis
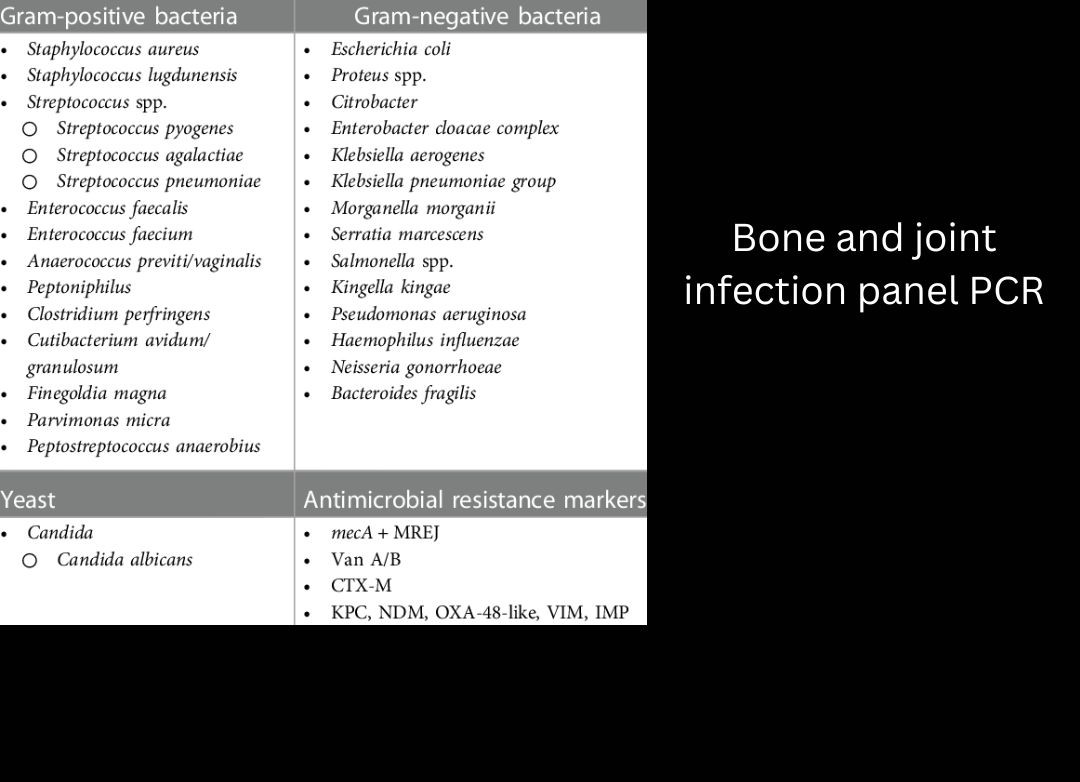
Raised inflammatory markers like ESR and CRP point towards infection but should be interpreted with caution in chronic infections. A normal level doesn’t rule out infection. Cultures from joint fluid or from the deep tissue are usually confirmatory but may be negative in presence of low virulent organisms and if the patient has received long term antibiotics beforehand. Newer diagnostic tools like BioFire Joint Infection Panel use PCR technique and are extremely sensitive. It identifies pathogens and antimicrobial resistance markers at the molecular level, encompassing the common causes of joint infections.It is not impacted by prior antibiotic use and targets difficult-to-grow organisms.
Treatment
A multidisciplinary approach is the key in managing bone and joint infections. The team includes (but is not restricted to) infectious disease physicians, microbiologists, orthopedic surgeons and plastic surgeons.
Host optimization: Irrespective of the nature of Bone/Joint infection presentation- host optimization remains a key step in achieving a successful outcome. Measures to optimize the host include- building up nutritional status, cessation of smoking and alcohol, control of blood sugar levels, stopping immunosuppressive medications etc.
PJI Prosthetic Joint Infection
Total hip and knee replacement are one of the most common orthopedic procedures performed these days. The numbers of patients receiving these procedures are estimated to rise by 150–600% for THA and TKA respectively by 2030 in the USA. Trends are similar in the rest of the world. Incidence of infection is around 1% for primary procedures and 5 % for revision surgeries. Prosthetic joint infection (PJI) is potentially the most significant complication following total joint arthroplasty. It is challenging for the surgeon to manage, physically and mentally disastrous for the patient and the cost to the health care system and society as a whole is high. For infections which are diagnosed early ( 3 weeks)- implant retention, debridement, exchange of modular components, and IV antibiotics may be tried. However, DAIR (Debridement, Antibiotics, Implant retention) has a success rate of around 50-60%.
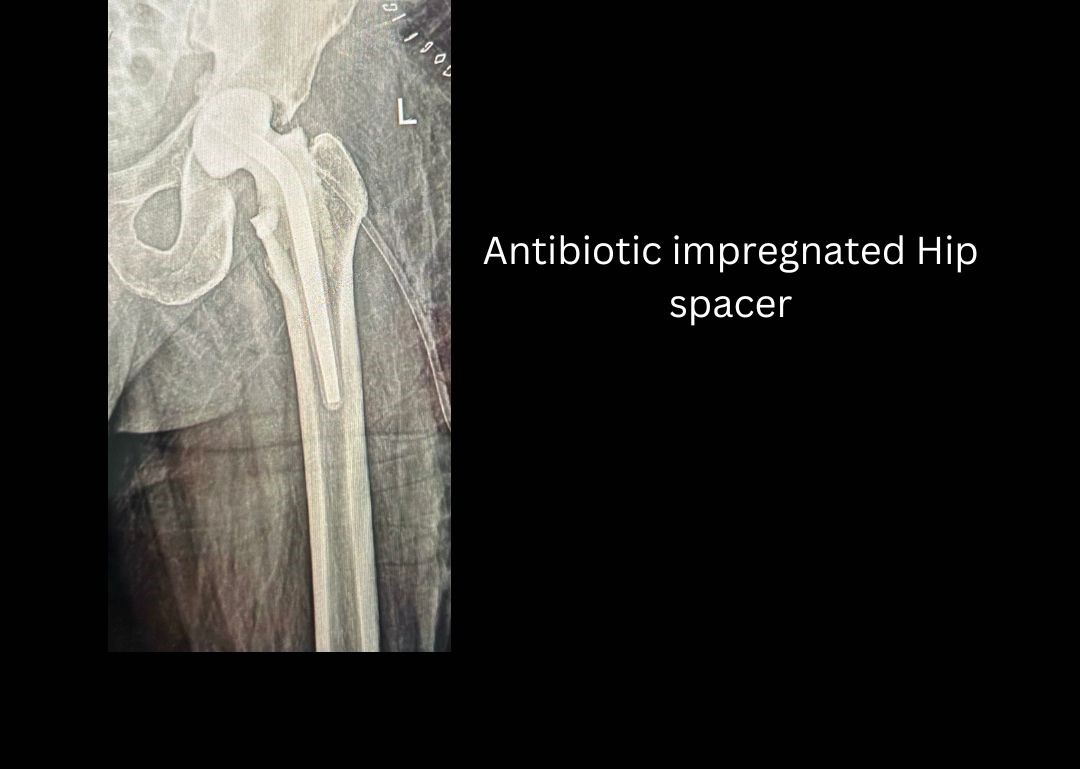
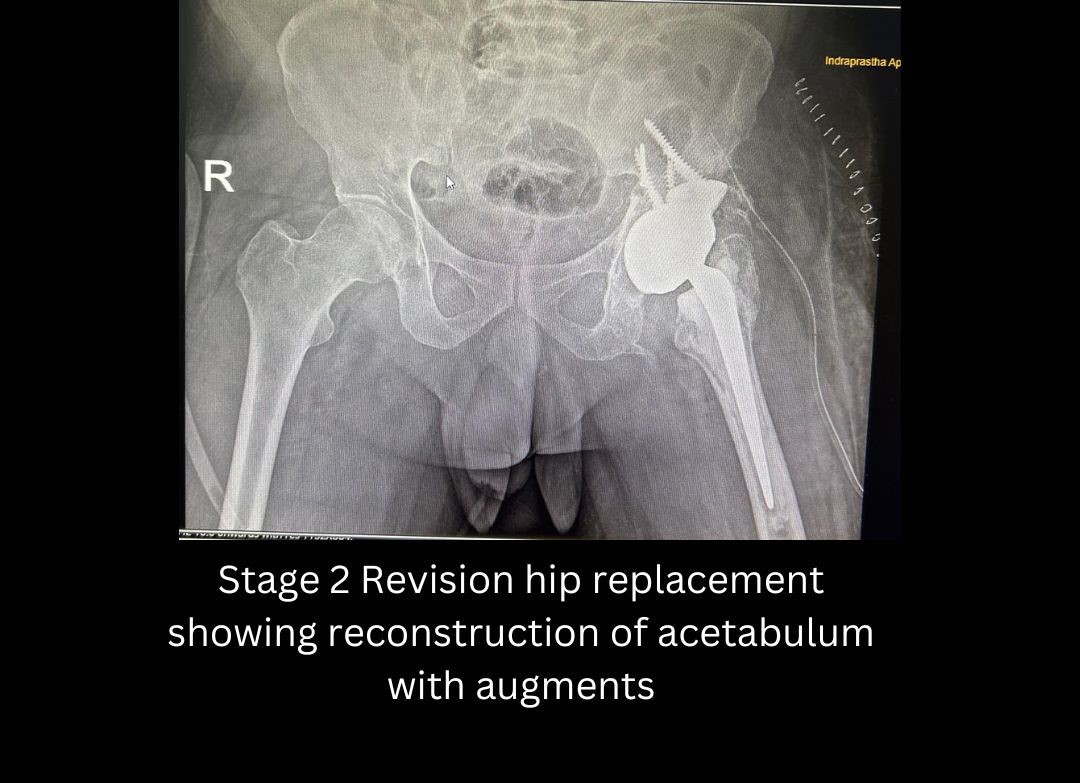
Two stage replacement is the gold standard for treatment of PJI. Stage 1 involves implant removal, debridement, placement of antibiotic cement spacer and culture specific antibiotics. Stage 2 is performed once the host bed is sterile as confirmed by negative synovial fluid cultures and inflammatory markers return to normal. Stage 2 involves reimplantation of the prosthesis. Single stage debridement and reimplantation although more convenient and appealing is advisable only under strict circumstances which include- infection by a known organism with low virulence and good antibiotic sensitivity, healthy soft tissues with no sinus tract, immunocompetent host, and absence of massive osteolysis.
FRI Fracture Related Infection
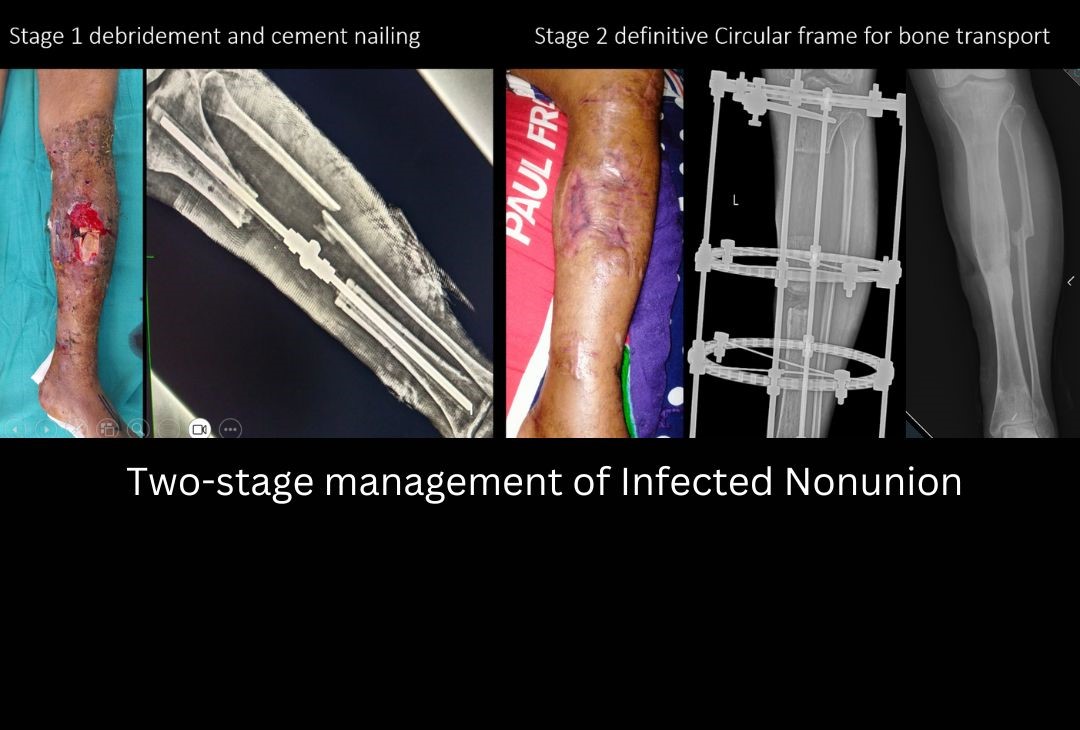
In contrast to PJI, FRI has received little attention until recently. Fracture-related infection is an infection involving a healed or unhealed bone fracture, whereby pathogenic microorganisms are present at any part of the fracture site, such as the involved bone, periosteum, surrounding soft tissues, adjacent joint, or (when present) the implant used for fixation. Infection does not rule out fracture healing- hence if there is adequate stability at the fracture site (no signs of implants loosening) and no gross sepsis- the implant may be retained along with debridement and suppressive antibiotics, in the hope of achieving fracture union. Achieving fracture union simplifies the management of FRI as then no foreign implant is needed to maintain fracture stability. Treatment of Infected nonunion on the other hand is one of the most challenging orthopedic problem. Principles of management of infected nonunion include:
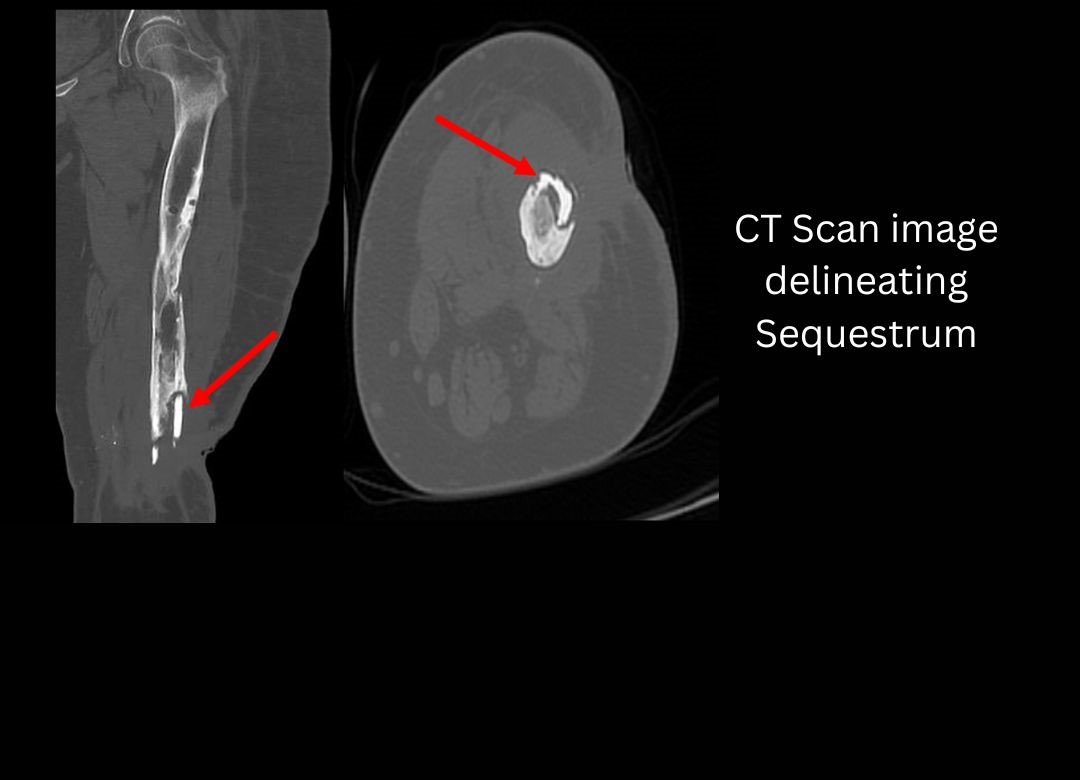
- Adequate and Judicious debridement- Identification and excision of all dead and necrotic tissue and bone (Sequestrum)
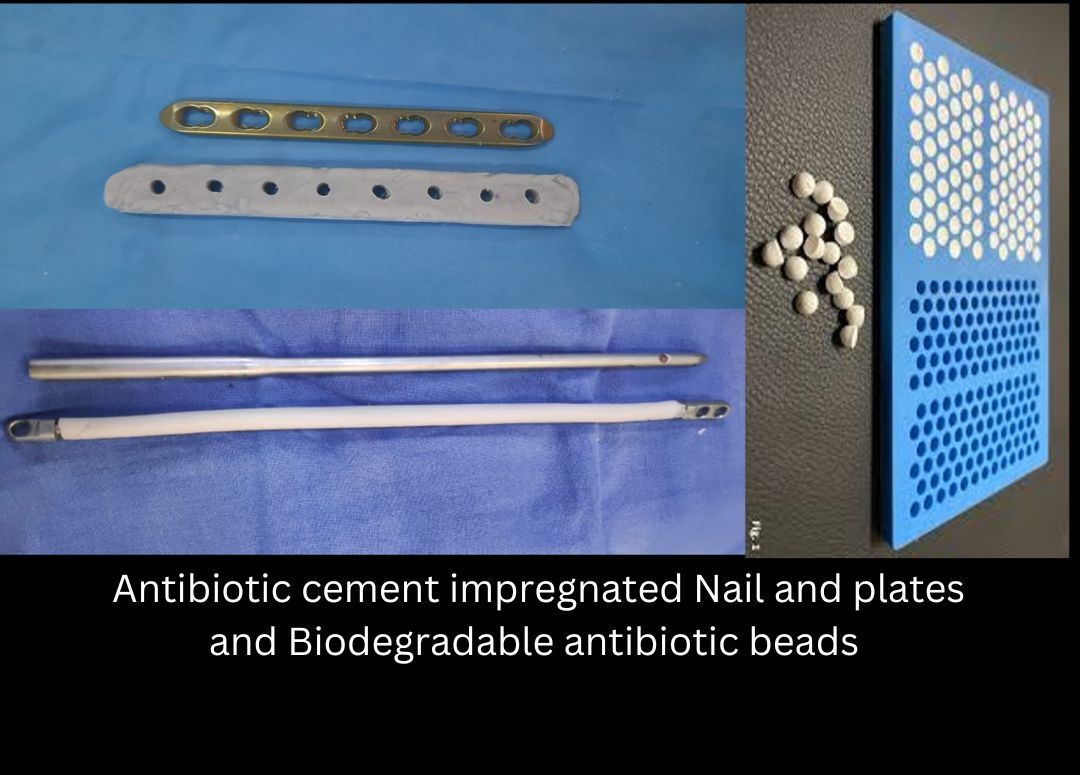
- Dead space management and local antibiotic delivery- the dead space created by debridement needs to be filled up. If not the ensuing hematoma forms an excellent culture medium for the residual micro-organisms after debridement. Dead space management can be done by various methods like- antibiotic cement beads, biodegradable antibiotic delivery beads, Antibiotic cement nails.
- Healthy soft tissue coverage
- Providing adequate fracture stability- Internal fixation with conventional plates and interlock nails in presence of infection is usually avoided. Fracture stability is provided by External fixators – like Monorail LRS or Circular Ilizarov type fixators. Antibiotic cement coated nails and plates can also be used as they provide both fracture stability and elute antibiotics locally and help to combat infection. Two stage treatment akin to PJI can also be used- wherein stage 1 involves implant removal, debridement, and temporary external fixation and stage 2 involves removal of External Fixator and placement of an Internal fixation device.
- Long term culture specific antibiotics.
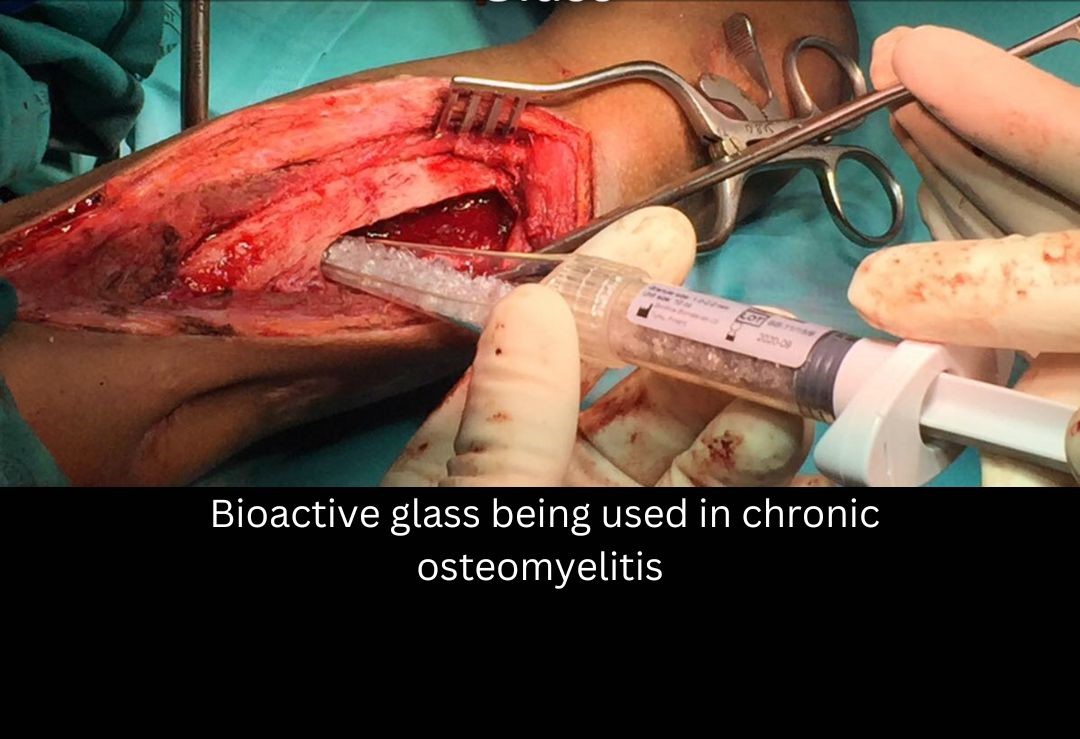
Chronic osteomyelitis
The incidence and prevalence of Chronic osteomyelitis has decreased over the years, as hygiene and sanitation measures have improved. However, it remains a challenging problem to deal with. Identification of dead and necrotic pieces of bone (known as Sequestrum) by CT scan is a crucial step . Surgical treatment involves removal of all sequestrum and filling the dead space with appropriate antibiotic delivery systems. Bioactive glass used as a dead space management agent has provided good long term results . It’s replaced by native bone gradually and has antimicrobial properties. The local vascularity may be enhanced by muscle flaps. Despite best efforts, cure rates in Chronic osteomyelitis are around 80%. Infections are recurrent especially in immunocompromised hosts.
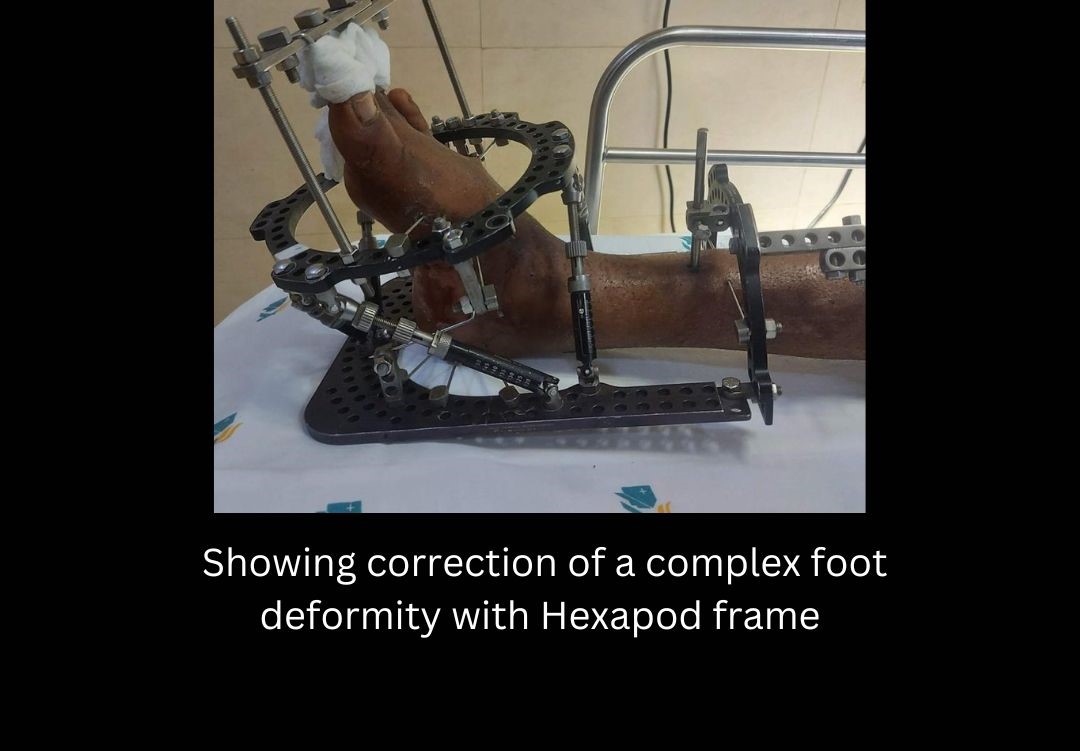
Diabetic Foot and Charcot Arthropathy
India is the world capital of Diabetes with maximum number of cases. Foot problems are common in patients with diabetes. They develop over time as the high blood sugar gradually damages the nerves and blood vessels in the feet. The nerve damage, called diabetic neuropathy, can cause numbness, tingling, pain, or a loss of sensation in feet. The loss or decreased sensation in the foot leads to increased risk of having a cut/blister or pressure ulcer as the patient is unaware. Such wounds get easily infected . The infection in turn may not heal well because the damaged blood vessels cause poor blood flow in the feet. Having an infection and poor blood flow can lead to gangrene. Many patients with diabetic feet end up in amputation if proper early care is not given. Extensive bony destruction in mid-foot area secondary to neuropathy can lead to rocker bottom feet and non-healing ulcers -known as Charcot foot deformities. Hexapod (TSF/TL Hex/ Deft Fix) is a very powerful tool which can help in management of such complex Charcot foot deformities. Correction of bony deformity allows the healing of soft tissue pressure ulcers as well.