Joint Replacement/ Arthroplasty- Hip and Knee
Joints especially hips and knees may be damaged due to degenerative disease like Osteoarthritis or inflammatory pathologies like Rheumatoid arthritis or by trauma. Advanced stages of arthritis require joint replacement/ arthroplasty. Modern day hip and knee implants have excellent longevity and provide good long term pain relief. Total joint replacement is one of the safest and most reliable treatments in any area of medicine. Pooled survivorship for Total Knee replacement implants is reported as 93.0% at 15 years, 88 % at 20 years, and 82.3% at 25 years. Whereas survivorship of hip prosthesis at 20 years is around 80%. With the advent of Highly Cross linked Polyethylene these survivorship statistics are expected to improve.
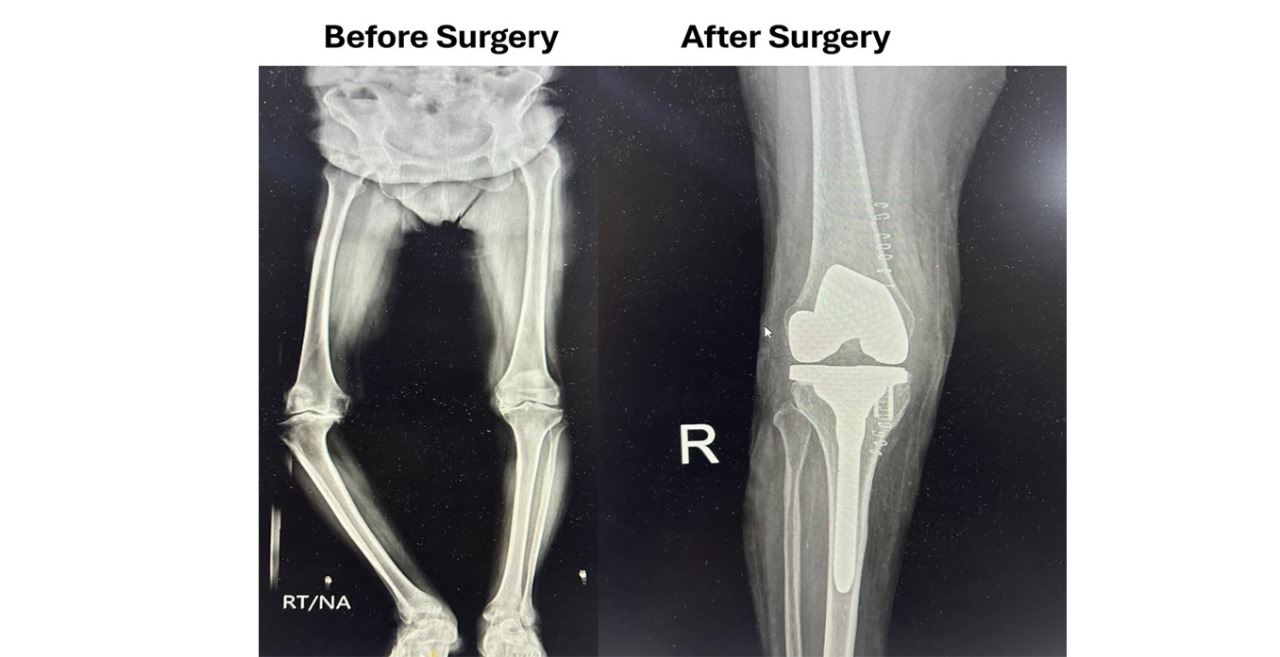
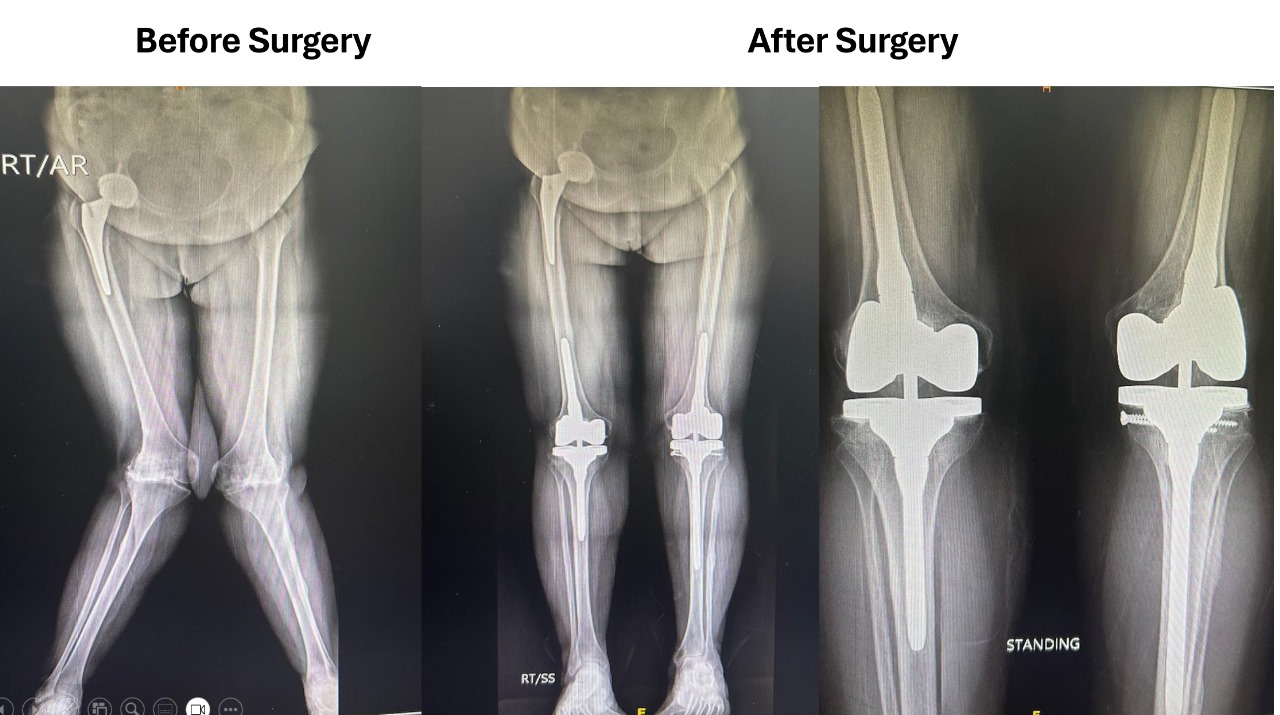
Total Knee replacement
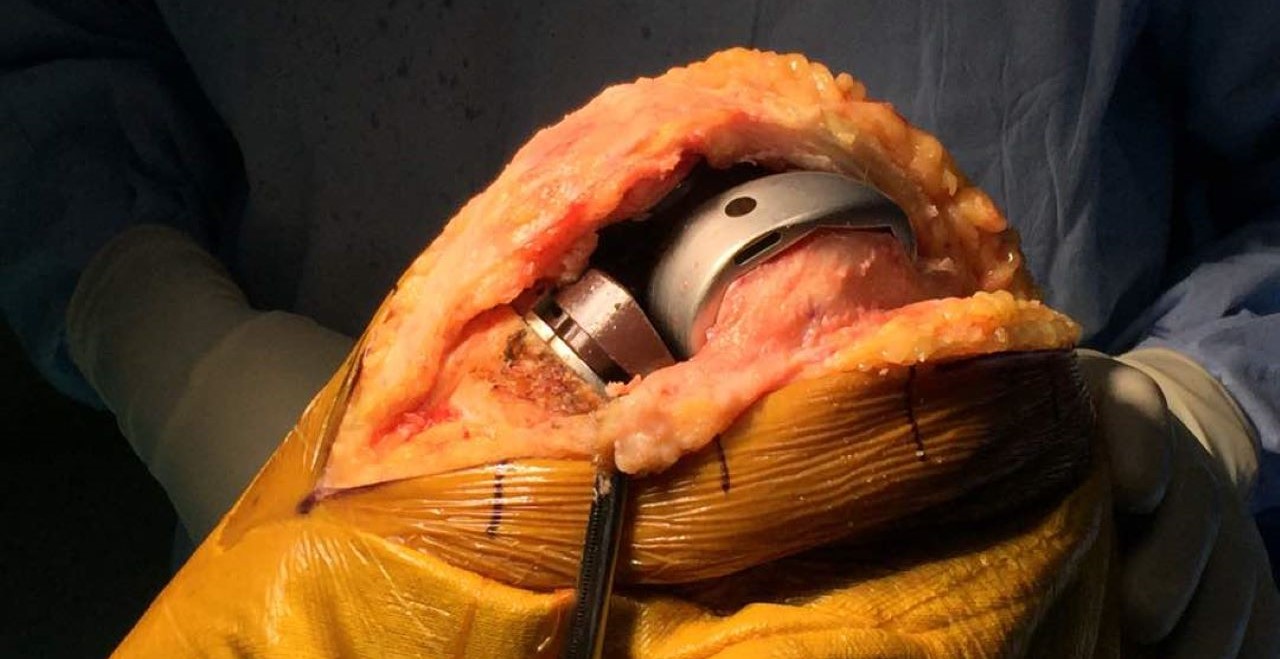
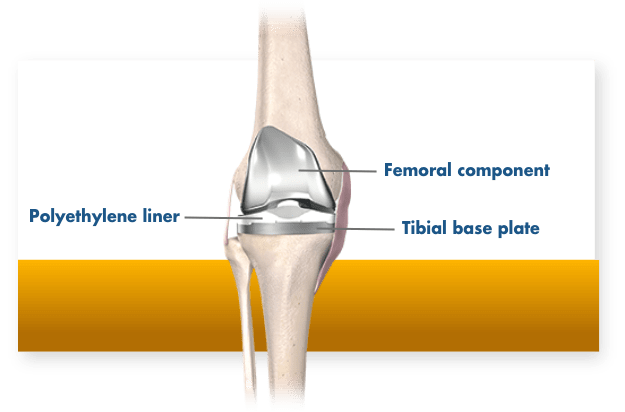
TKR involves replacing the damaged arthritic surfaces of distal femur and proximal tibia with metallic prosthesis and a polyethylene spacer interposed in between the metallic component. There are three types of implants available: Cruciate Retaining, Cruciate Sacrificing and Posterior Stabilized Knee joints. The choice of implant to be used depends upon many factors- like the amount and type of deformity, age, size of the implant and surgeon preference. The material used in knee implants is usually either Cobalt -Chromium alloy or Titanium. In patients who are allergic to these metals- Oxinium or gold coated implants are an attractive alternative. Fixation of the implants to the bone is done using bone cement. The goal of knee replacement is to provide long term pain relief and correct the limb alignment.
Unicondylar knee replacement (UKR) involves replacing only the damaged medial half of the knee joint. This surgery is much smaller than a conventional Total knee replacement and has better return to function. The recovery is quicker and much better as all the native ligaments are retained. The surgical incision, post operative pain and blood loss are much lower. It is done in patients with uni-compartmental arthritis.
Robotic knee replacement involves the use of robotic assisted arm which helps to increase the accuracy of bone cuts while performing the knee replacement surgery. A preoperative CT scan is usually required which is then used to create a virtual 3-dimensional model of the patient’s knee. Implant sizing and cuts are then planned preoperatively and adjusted intraoperatively based on the bony deformity and ligamentous laxity. Any patient who is a candidate for knee replacement can undergo a robotic knee surgery. However Robotic technology is especially useful in pre op planning and intra op execution of complex challenging cases – severe deformities, Extra articular deformities, pre-existing hardware around knee. Robotic-assisted knee replacement surgery is not done by a robot alone. Instead, it acts as a guide, helping the surgeon to follow the plan laid out in advance. Like during traditional surgery, the orthopedic surgeon is in control, however, we use the robot as an additional surgical tool. The robot enhances the surgeon's skills during some stages of the surgery to help deliver the best possible outcomes.
Complications: Although knee replacement is extremely safe, yet complications are possible as in any surgical procedure. Potential complications of knee replacement include Infection, Aseptic loosening, Patellar complications, Periprosthetic fractures, Deep vein Thrombosis and Pulmonary embolism.
Total Hip Replacement
Total hip replacement involves replacements of the ball (femoral head) and Socket (Acetabular) component of the hip joint. The hip joint may be destroyed secondary to osteoarthritis, inflammatory arthritis (Rheumatoid Arthritis), avascular Necrosis or post trauma. When destruction of the hip joint is severe and irreversible- total hip arthroplasty provides a reliable pain free surgical option. Hip replacements are known to improve patient quality of life more than any other elective procedure. Between 2018 and 2050, primary hip replacement is predicted to increase by between 41.9% and 114.3% in France, and by 174% between 2005 and 2030 in the USA. Partial Hip replacement involves replacement of only the femoral head component and is usually done on cases of Fracture neck of femur in elderly people.
The prosthetic components may be fixed to the host bone with cement or press fitted (Uncemented). Uncemented and Cemented Femoral stems have different designs- cemented stem are smooth and polished, whereas uncemented stems are rough and coated. Uncemented fixation is gaining popularity and is suited for relatively younger individuals with good quality bone. Cemented fixation (especially femoral stem) on the other hand is preferred in elderly patients with osteoporosis and wide medullary canals. Uncemented Cup placement involves placement of metallic shell- which is press fitted in the acetabular bone socket, followed by insertion of a polyethylene/Ceramic liner which is locked in the metal shell. Cemented cup placement on the other hand involves direct placement of a Polyethylene cup inside the Acetabulum which is fixed with the help of bone cement.
Following placement of femoral stem and acetabular cup, a prosthetic femoral head is placed over the stem and hip joint is then reduced and checked for limb length and stability. Femoral heads may be metallic or ceramic. Wear rates of metallic head with polyethylene liner have traditionally been higher as compared to Ceramic heads with Ceramic liner or polyethylene liner. Hence Ceramic heads with Highly cross-linked polyethylene liners are usually the preferred bearing surfaces.
What is Hip Replacement?
Dual Mobility cups: Dual Mobility is newer type of prosthetic hip design which promises to provide better range of motion and lessen the risk of dislocation. Compared to a traditional prosthesis for a hip replacement, a dual mobility implant provides an additional bearing surface (it has an inner ceramic or metal head and a bigger outer polyehylene head). With the dual mobility hip, a large polyethylene plastic head fits inside a polished metal hip socket component, and an additional smaller metal or ceramic head is snap-fit within the polyethylene head. Dual mobility cups are better suited for individuals with higher risk of dislocation and young patients who put a lot more stress on the hip prosthesis.
Anterior or Minimally Invasive Hip replacement: The traditional hip replacement is done through a posterior or lateral approach and utilizes a relatively larger skin incision. Minimally invasive THR is usually done through the front (anterior) of the hip and involves a smaller incision. Minimally invasive techniques may not, however, be suitable for all patients. The implants used are the same as those used for traditional hip replacement. However, specially designed surgical instruments are needed to prepare the socket and femur and to place the implants properly. Minimally invasive techniques may be less suitable or create a higher risk of complications for patients who: are overweight, have already undergone other hip surgeries, have a significant deformity of the hip joint, are very muscular or have health problems that may slow wound healing. The benefits of minimally invasive hip replacement have been reported to include less damage to soft tissues, leading to a quicker, less painful recovery and more rapid return to normal activities. Current evidence suggests that the long-term benefits of minimally invasive surgery do not differ from those of traditional hip replacement.