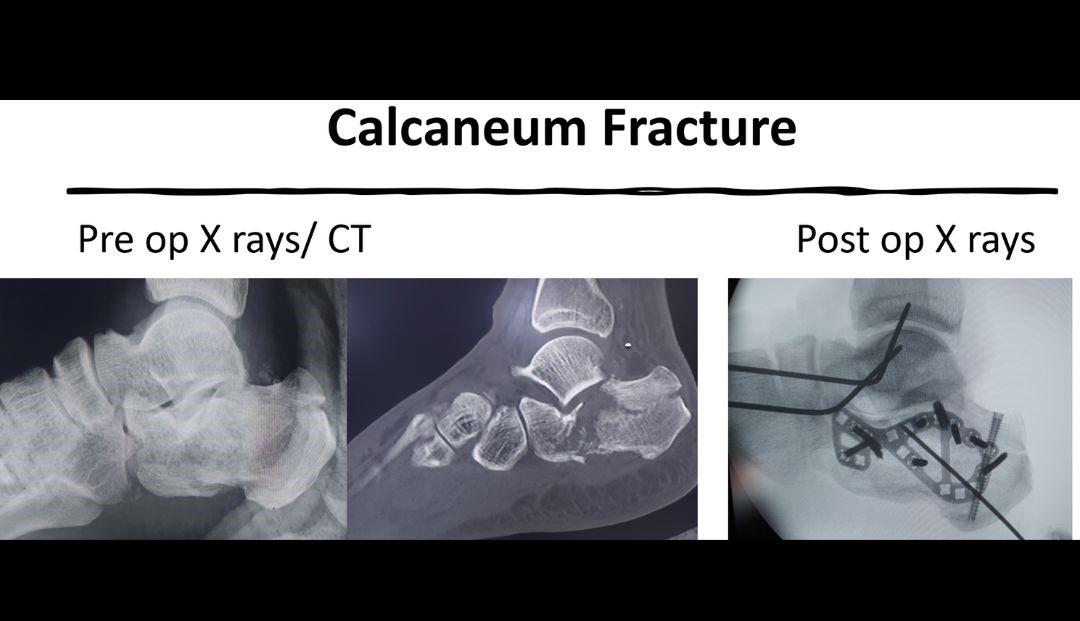
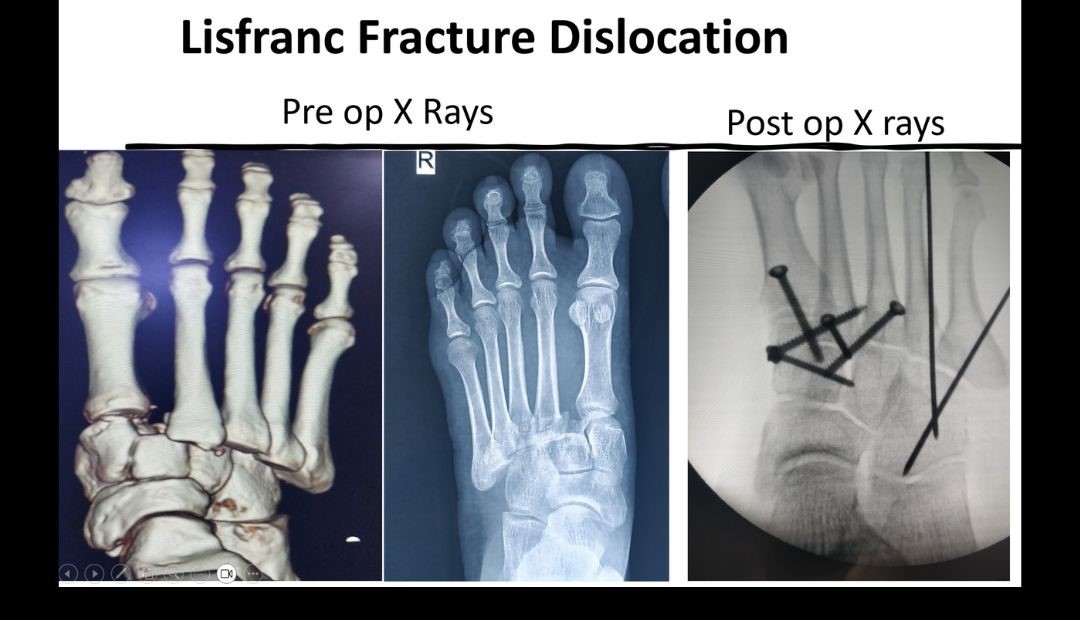
Trauma/Fractures
The human foot is a highly developed, biomechanically complex structure that serves to bear the weight of the body as well as forces many times the weight of the human body during propulsion. The foot itself can be divided into 3 parts: the hindfoot, the midfoot, and the forefoot. The hindfoot is composed of 2 of the 7 tarsal bones, the talus, and the calcaneus; the midfoot contains the rest of the tarsal bones; and the forefoot contains the metatarsals and the phalanges. Foot has 26 bones and 33 joints which can be injured during various activities. Treatment for a foot fracture depends on several factors, including: which bone(s) are fractured, the type of fracture, the severity of your fracture.
DEFORMITY
Foot and ankle region can be affected by various deformities. One significant aspect of foot structure is the arch, which refers to the curve along the bottom of the foot. A normal arch is often considered the ideal foot type, where the arch has a moderate curve and provides a balanced distribution of weight across the foot. This arch type is associated with good stability and proper shock absorption, reducing the risk of foot problems. A low arch, also known as a flat foot / Planovalgus , is characterized by a minimal or no visible arch. This foot type tends to roll inward excessively (overpronation) during walking or running, leading to instability and an uneven distribution of forces. People with flat feet may experience issues such as foot fatigue, shin splints, and Achilles tendonitis.
Some of the treatment options for painful flatfeet are:
- Arch supports (orthotic devices): Hard Arch supports can help relieve the pain caused by flatfeet. Sometimes custom-designed arch supports that are molded to the contours of the feet are recommended. Arch supports won't cure flatfeet, but they often reduce symptoms.
- Stretching exercises: Some people with flatfeet also have a shortened Achilles tendon. Exercises to stretch this tendon may help.
- Physical therapy: Flatfeet may contribute to overuse injuries in some runners. Exercises to strengthen the muscles and tendons in the feet and guidance to improve gait.
- Surgery: Surgical options for treating flat foot depends upon the cause of flat foot. In flexible flatfoot, the arch is formed normally on toe standing. Such cases may benefit from placement of a screw or device to block eversion at the subtalar joint. Other options include Calcaneal osteotomies and ligament reconstructions. In adults the tibialis posterior tendon is addressed along with Tendo Achillis lengthening. Severe cases with arthritis may require triple arthrodesis.
Cavus Foot Or High arch feet may be genetic, or they may be caused by a number of underlying conditions. People with high arches may experience pain, and in some cases, permanent damage to their foot structure. There are several treatments available, including orthotics, splints, physical therapy and surgery. Charcot-Marie-Tooth (CMT) disease is an inherited disorder that causes smaller, weaker muscles. High arch feet are common among people with this disorder.
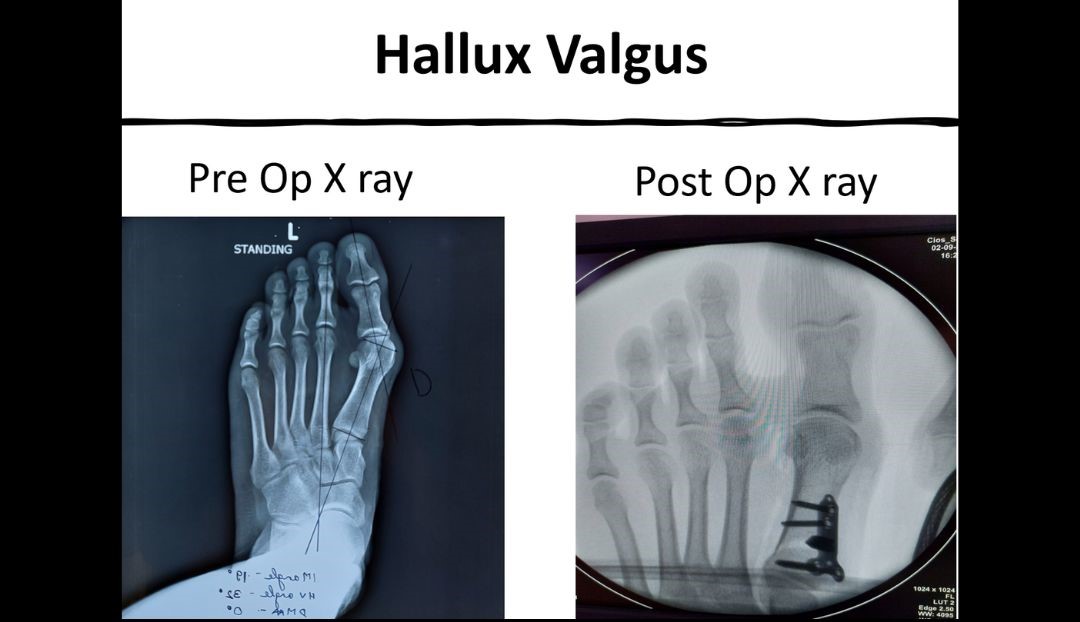
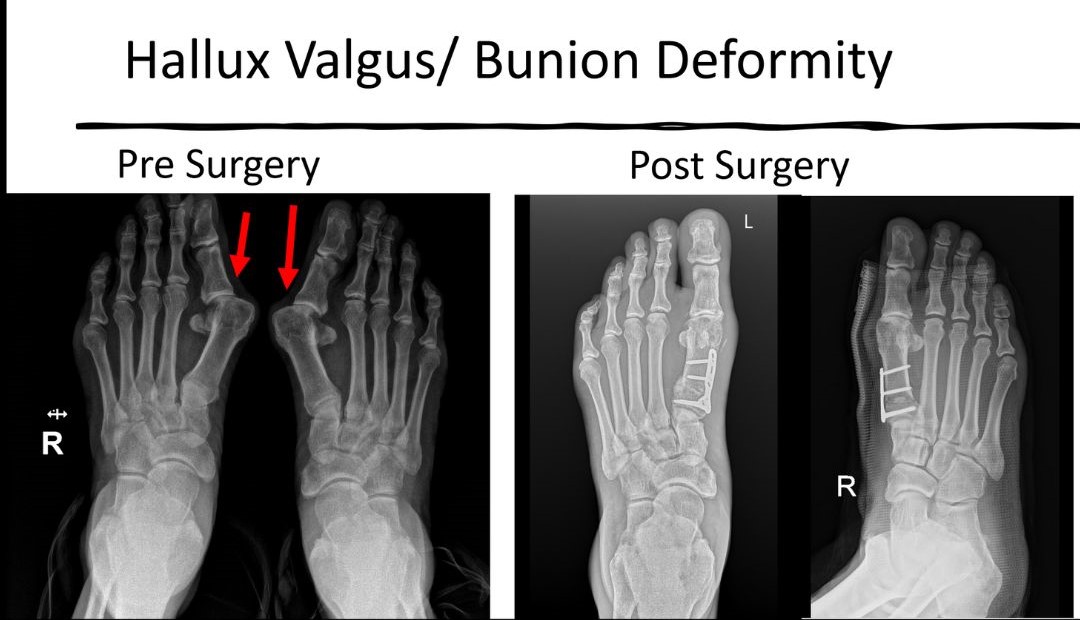
Hallux Valgus/Bunion: A bunion is a bony bump that forms at the base of your big toe. Bunions develop on the inside edge of your big toe joint — the metatarsophalangeal (MTP) joint. Apart from the deformity bunion can cause other symptoms, including- Pain or stiffness, swelling, discoloration or redness, an inability to move or bend your big toe, difficulty wearing certain types of shoes, or pain that gets worse when you’re wearing shoes, Corns or calluses, Hammertoes (painful, tight toe tendons and joints).
The most common bunion treatments include:
- Footwear changes: Switching to shoes with wide, deep toe boxes can take pressure off your toes. You may be able to use a stretching device to widen shoes you already own.
- Bunion pads and taping: Over-the-counter (OTC) bunion pads cushion the area around a bunion to relieve pressure. Your provider might suggest using medical tape to hold your toes in the correct position.
- Pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce pain and swelling.
- Icing: TApplying ice or cold packs to your affected toe may also help. Wrap a cold pack in a thin towel to avoid putting it directly onto your skin.
- Physical therapy: You may need to work with a physical therapist to strengthen your foot. They’ll give you exercises or stretches that may help your toes stay in better alignment.
- Surgery: Surgery can correct deformity and is a treatment options when conservative options fail or when the deformity is severe.
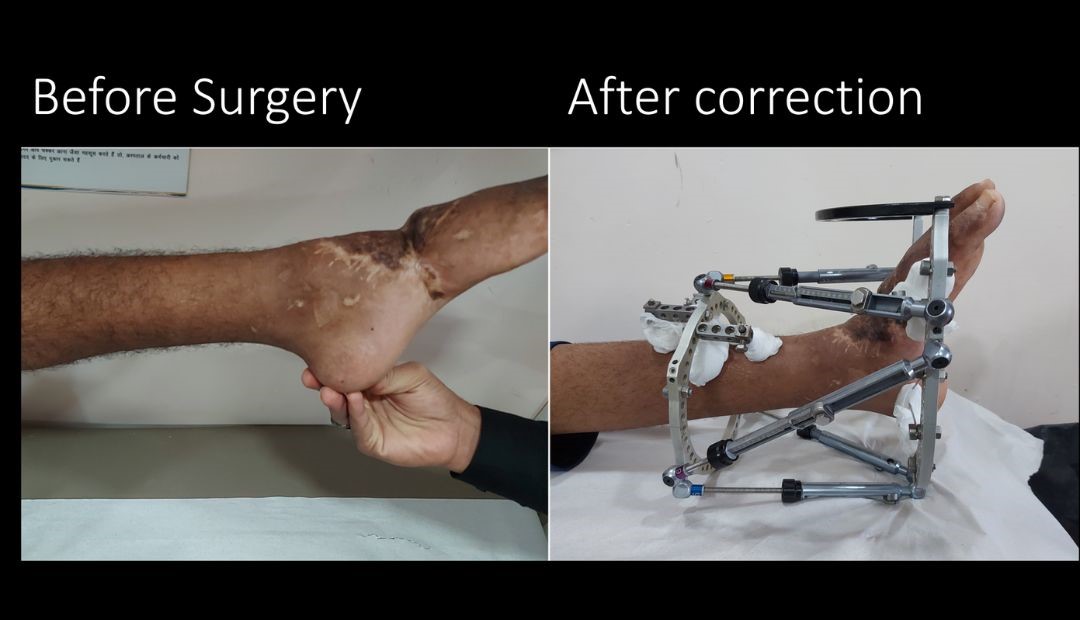
Complex deformities: complex deformities may be the result of trauma or neurological disorders. They are severe and often require surgery. A sensate foot is a prerequisite for performing deformity correction surgery. Complex deformities usually require joint fusion and a stable plantigrade painless foot is the aim.
SOFT TISSUE INJURIES
The foot and ankle is supported by many important ligaments and tissues which may get injured or inflamed.
Ankle sprains are common injuries that occur among people of all ages and at all activity levels; in fact, they are the number one reason for missed participation in athletics. An ankle sprain occurs when the strong ligaments that support the ankle stretch beyond their limits and tear. Most sprains heal with conservative treatments like ice, elevation, over-the-counter medications, and simple rehabilitation exercises. If symptoms do not improve despite non-operative treatment, surgery may be need to repair or reconstruct the injured ligaments.
Without proper treatment and rehabilitation, a chronic or untreated severe sprain can weaken the ankle, making it more likely that it will injure it again. Repeated ankle sprains can lead to long-term problems, including chronic ankle pain, arthritis, and instability.
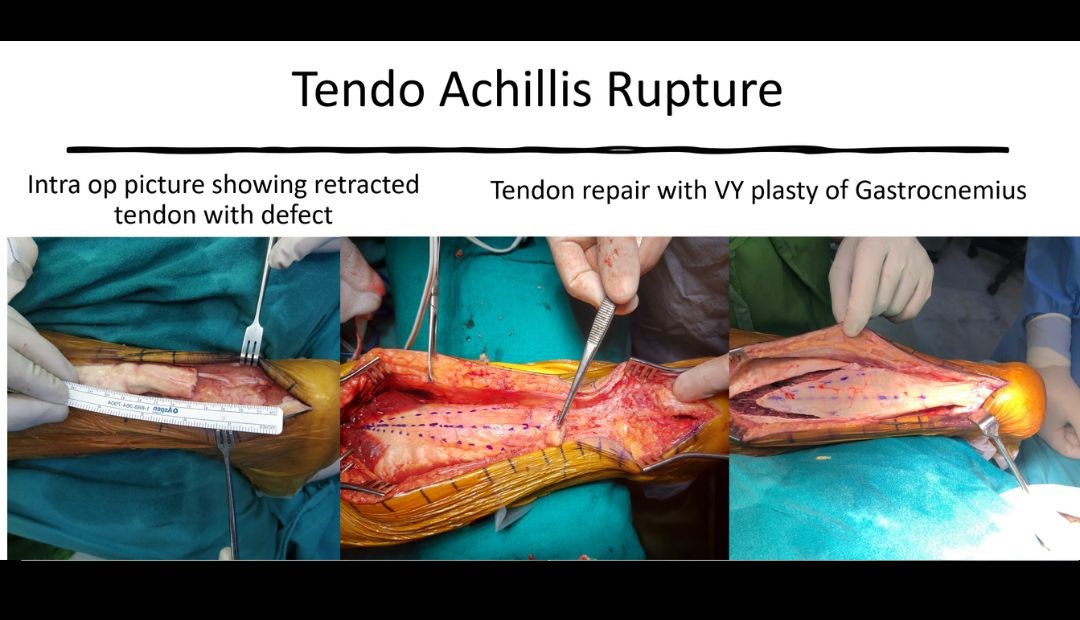
Tendo Achillis rupture: The Achilles tendon is a strong fibrous cord that connects the muscles in the back of calf to heel bone. Achilles Tendon Ruptures are common tendon injuries that occur due to sudden dorsiflexion of a plantarflexed foot, most commonly associated with sporting events. Diagnosis can be made clinically with weakness of plantarflexion with a positive Thompson's test. MRI studies may be indicated for surgical management of chronic injuries. Treatment may be nonoperative or operative depending on patient age, patient activity demands and chronicity of injury. The injury may be missed in up to 25%. Its more common in men between ages of 30-40 years. Risk factors include episodic athletes, flouroquinolone antibiotics and local steroid injections.
Plantar fasciitis: It is one of the most common causes of heel pain. It involves inflammation of a thick band of tissue that runs across the bottom of each foot and connects the heel bone to the toes, known as the plantar fascia. Plantar fasciitis commonly causes stabbing pain that often occurs with your first steps in the morning. As you get up and move, the pain normally decreases, but it might return after long periods of standing or when you stand up after sitting. The most common treatments for plantar fasciitis include:
- NSAIDs: NSAIDs (like aspirin, ibuprofen and naproxen, rest, icing your foot)
- Wearing supportive shoes:Wear sturdy, well-cushioned shoes. Don’t wear sandals, flip-flops or other flat shoes without built-in arch support. Don’t walk with bare feet.
- Orthotics or shoe inserts: You can add inserts into your shoes that add extra arch support. Your provider will suggest either pre-made inserts you can buy over-the-counter or custom-made orthotics that are molded to the exact shape of your foot.
- Immobilization: Wearing a walking boot (sometimes called a walking cast or a pneumatic cam walker) for a few weeks will hold your foot in place and take pressure off your plantar fascia.
- Massaging and stretching: Stretches and massage techniques can help decrese the pain in the foot.
- Corticosteroids:Massaging and stretching: Corticosteroids are anti-inflammatory medicines. Injecting a corticosteroid (like prednisone) into the plantar fascia decreases the inflammation.
- Platelet rich plasma (PRP):PRP is usually injected to heal and repair injuries.
- Percutaneous needle tenotomy: During a percutaneous tenotomy, a needle is used to puncture through the skin into the plantar fascia. The body sends more blood than usual to the area, which then stimulate the plantar fascia’s ability to repair itself.
Plantar fasciitis surgery
The treatments listed above are usually all you’ll need to relieve your symptoms and treat plantar fasciitis. It’s very rare to need surgery. The two most common types of surgery include:
- Gastrocnemius recession:This surgery will lengthen your calf muscles to reduce pressure on your plantar fascia.
- Plantar fascial release:It involves making tiny incisions (cuts) in your plantar fascia to relieve some of the extra tension.
Neurological disorder of foot:
Charcot foot: India is the world capital of Diabetes with maximum number of cases. Foot problems are common in patients with diabetes. They develop over time as the high blood sugar gradually damages the nerves and blood vessels in the feet. The nerve damage, called diabetic neuropathy, can cause numbness, tingling, pain, or a loss of sensation in feet. The loss or decreased sensation in the foot leads to increased risk of having a cut/blister or pressure ulcer as the patient is unaware. Such wounds get easily infected. The infection in turn may not heal well because the damaged blood vessels cause poor blood flow in the feet. Having an infection and poor blood flow can lead to gangrene. Many patients with diabetic feet end up in amputation if proper early care is not given. Extensive bony destruction in mid-foot area secondary to neuropathy can lead to rocker bottom feet and non-healing ulcers -known as Charcot foot deformities. Hexapod (TSF/TL Hex/ Deft Fix) is a very powerful tool which can help in management of such complex Charcot foot deformities. Correction of bony deformity allows the healing of soft tissue pressure ulcers as well.
Tarsal tunnel syndrome: The tibial nerve in ankle runs through your tarsal tunnel, a passage made up of bones and ligaments. People who have TTS may have pain, tingling, numbness or weakness in their feet. You’re more likely to develop TTS if you exercise strenuously or frequently, especially if you have a very flat foot. Treatment for TTS includes- rest, ice packs, Anti-Inflammatory medications, Orthotics and support, physical therapy and exercises and corticosteroid injections. Surgery to decompress the nerve and the tarsal tunnel amy be needed if conservative measures fail.
Morton neuroma: Morton's neuroma is a painful condition that affects the ball of foot, most commonly the area between the third and fourth toes. Morton's neuroma may feel as if one is standing on a pebble in your shoe or on a fold in your sock. This can cause a sharp, burning pain in the ball of the foot. It may lead to stinging, burning or numbness in the affected toes. High-heeled or tight shoes have been linked to the development of Morton's neuroma. People who have bunions, hammertoes, high arches or flatfeet are at higher risk of developing Morton's neuroma. Many people experience relief by switching to lower heeled shoes with wider toe boxes. Sometimes corticosteroid injections or surgery may be necessary.